What Are Eating Disorders?
Eating disorders include obesity, bulimia, anorexia and binge eating. They are characterized by an abnormal consumption and relationship to food: overeating beyond the natural mechanism of hunger and satiety, purging with excessive dieting, over-exercising or vomiting, cravings and aversion to food. Eating disorders have an obsessive-compulsive component and use the same biological pathways as drug addiction: the reward system of the brain.
When food becomes a substance of abuse in the same way cocaine is, treatment must include a quantum transformation of the mind, from addiction to awareness. Non-judgmental observation of one’s thoughts, feelings, sensations or mindfulness is a successful method to deal with cravings and aversion to food and prevent relapse in the recovering patient.
Prevalence
The most prevalent eating disorder is bulimia. It is about four times more frequent than anorexia. It affects mostly young women between the ages of 12 and 25. Only 10 -15 % of those with bulimia and anorexia are men. Eating disorders have the highest mortality rate of all mental illnesses, 50% meet the criteria of depression and only one in ten receive treatment. Eating disorder statistics provided by the National Eating Disorder Association indicate that 10 million American women suffer from eating disorders and 61% of American adults are either overweight or obese.
Natural Mechanism of Hunger and Satiety and the Dopamine Reward System
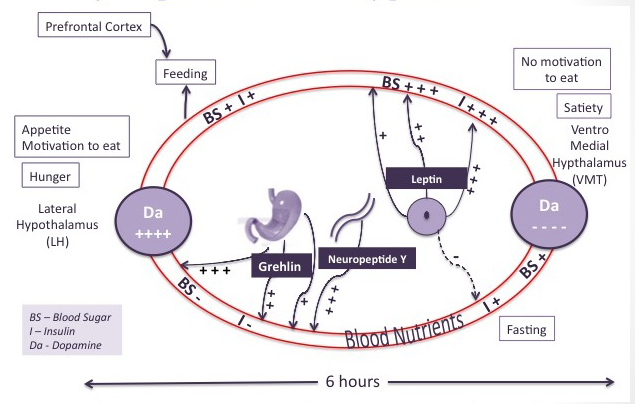
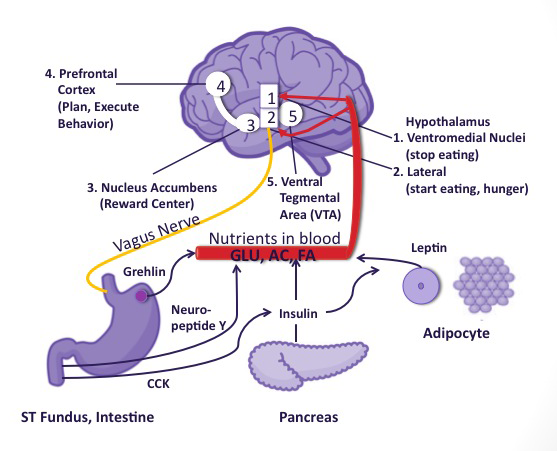
Nature provided us with a basic biological mechanism for individual survival. This system consists of a set of hormonal secretions signaling hunger, satiety and pleasure. When four hours or so have passed after eating, the stomach is empty. Blood sugar and insulin levels are low and feeding is necessary to provide energy to the body. Low blood sugar stimulates the secretion of Ghrelin by the stomach, the hunger hormone, which in turn stimulates the secretion by the hypothalamus of neuropeptide Y, the greatest appetite stimulant. Ghrelin also stimulates the production of dopamine in the hypothalamus. Increasing levels of dopamine causes the motivation to eat, or appetite.
In normal circumstances, the motor cortex is activated and the eating behavior follows. With food intake ghrelin secretion decreases while insulin and leptin secretion increase. Leptin is the satiety hormone secreted by adipose tissue. The secretion of insulin and leptin signals that sufficient food storage has taken place. High insulin levels suppress dopamine-producing neurons, and stimulate serotonin secretion. Appetite is suppressed, satiety is achieved, the food does not look appealing anymore and the feeding behavior is terminated.
Disturbances of the Dopamine Reward System in Anorexia and Binge Eating Disorders
Studies show that anorexia is associated with increased dopamine receptors in the brain and low motivation to eat. On the contrary, research shows that obese and binge eating individuals produce a lesser amount of dopamine during the feeding period, therefore needing more food to attain the pleasure satiety threshold. More recent studies conducted by the University of San Diego show an abnormal psychological response by anorexics to the stimulation of the dopaminergic system. Instead of experiencing pleasure with increased levels of dopamine, anorexics experience anxiety. This abnormal response to dopamine secretion would be the biological basis for the lack of feeding.
Opiates and the Reward System
Fatty, sugary foods release opioids in our bloodstream that binds to the same opiate receptors that get activated with opiate drugs. When these receptors are activated we have a feeling of pleasure and elation. This is the way nature wired our brain to make us perform activities essential to survival: drinking, eating and sex.
Role of Serotonin, Cortisol and Sex Hormones
Low serotonin levels have been found in the brain of bulimics and people suffering from a binge eating disorder. Binging may be an attempt to increase serotonin levels to reach satiety. On the opposite end, anorexia is associated with high serotonin levels and food abstinence may be the consequence of feeling satiated and lacking appetite. High serotonin levels produce an uncomfortable jittery sensation in the body and food abstinence may be the attempt to get rid of this feeling.
Cortisol, the stress hormone produced by the adrenal glands has been found to be chronically elevated in bulimia and anorexia suggesting an imbalance between the sympathetic (alertness) and parasympathetic (relaxation) systems.
Hypothalamic disturbance include sex hormone disruptions that cause amenorrhea or the absence of menstrual cycle.
Hunger, Appetite, Stomach Hunger and Brain Hunger
Hunger and appetite are the biological and psychological expression of the need to eat to survive. The center of hunger and appetite is in the hypothalamus and it is connected to the prefrontal cortex area that tells us what we need and want. Hormones, neurotransmitters and the vagus nerve regulate hunger and appetite. The vagus nerve (see illustration of vagus nerve and brain below) transmits messages from the gut to the brain. This efficient survival mechanism has protected us from starvation when food supply was scarce or intermittent. Our brain is wired to prefer high fat and high sugar foods that our body stores as fat to be used in periods of famine. Today, in a world of plenty, this mechanism has been high jacked by the food industry and has become a curse leading to obesity and eating disorders.
Modern food industry, artificially combining highly desirable high sugar and high fat in food products, produces unprecedently rewarding foods for the brain. For instance, some substances such as High Fructose Syrup act in the same way as addictive drugs. It is immediately absorbed in the blood and produces a buzz, a high, a strong pleasure and a feel good sensation. The brain creates an association between that food and a high level of pleasure. In times of low blood sugar, stress or emotional hardship, the brain remembers the effects of that food and sends us a message that it wants it. This is brain hunger.
Cravings: How They Work
The term ‘craving’ has been defined as a motivational state characterized by an intense desire or urge for a particular substance, usually drugs or food (Cepeda-Benito, Gleaves, Williams, & Erath, 2000). In eating, food cravings are specific and necessitate prior exposure to the food item desired and craved. Cravings involve the imagery of very specific foods: greasy potato chips or extra sweet ice cream, high in sugar and fat. In times of stress or dietary restriction, the brain as a quick fix for reestablishing hormonal or emotional homeostasis recalls these foods. For the most part, cravings are independent of hunger and appetite and are a response to emotional distress. Mental imagery is central to the compelling desire for that food. Research has shown that visual imagery causes the salivary glands to produce saliva and an increase of dopamine in the brain. Recent research shows that cravings may be a response to a deficiency of serotonin and dopamine. Cravings can lead to a compulsive need to binge in individuals affected by bulimia or obese people.
Psychological and Social Factors
Control of the internal environment is a central issue for bulimics and anorexics. Manipulating food intake becomes synonymous with controlling feelings. The brain learns to deal with emotional stress by manipulating eating behaviors. Purging can be a strategy to manage anxiety or uncomfortable feelings. Purging can also be a way to deal with loneliness or lack of purpose.
Controlling body weight is another major issue. Anorexics see themselves as overweight, although they may be skin and bones. They usually suffer from poor self-esteem, obsessive-compulsive behavior, anxiety and depression.
Often, bulimics and anorexics have a family history of eating disorders and have suffered from childhood trauma and abuse. The increasing number of eating disorders in adolescents is central to a culture that promotes thinness in magazines and TV, as a way to achieve happiness, beauty and attractiveness.
Consequences of Eating Disorders
Bulimics may suffer from vomiting related problems such as tooth decay, Barrett’s esophagus (a serious complication of GERD which can lead to esophageal adenocarcinoma) and nutritional deficiencies. The nature of their disorder leads them to social isolation and with difficulty in finding intimacy in their relationships.
We have found that some patients change their eating behaviors over time in an attempt to heal. For instance, someone will start with anorexia and few years later move to bulimia and then to overeating or over-drinking or abusing drugs. Recent research (Brookhaven National Laboratory) shows a similarity between the brains of drug addicts and those who are obese with strong food cravings. Neuroimaging studies show that loss of control overeating and obesity produces changes in the brain similar to those produced by drug abuse. “Food, highly palatable and energy dense, has become a substance of abuse.” Eating disorders, Overeating and Pathological Attachment to Food: Independent or Addictive Disorders”, Mark S. Gold, MD.
Obesity is the consequence of overeating and chemical dependency on food. Eating disorders are serious illnesses that are difficult to treat and they deserve full attention from family and friends.
Addictive Foods
Addictive foods: sugar, chocolate, cheese and meat have a special effect on the brain, similar to a drug. They create an out of control feeling in the food addict and dependence similar to drug addiction. Addictive foods stimulate the opiate reward system of the brain increasing pleasure.
“[These foods] contain chemical compounds no one ever suspected were there—mild opiates that are released during digestion. Other researchers have added evidence that there really is something about sugar, chocolate, cheese, meat and certain other foods that sets them apart. They don’t just tickle the taste buds. It appears they actually stimulate the brain in such a way that it is easy to get hooked and tough to break free, even if you find yourself gaining weight or lapsing into health problems.” Breaking the Food Seduction: The Hidden Reasons Behind Food Cravings—and 7 Steps to End Them Naturally, Neil Bernard, M.D..
“When the sugar-sensitive person tries to stop using the sugar that evokes this wonderful beta-endorphin response, the receptors start screaming. This is called withdrawal. The person experiencing withdrawal may feel cranky, irritable, and out of sorts but never knows it was last night’s sugar binge creating the horrible feelings. Cravings loom large as the beta-endorphin receptors scream and relief is as close as a can of soda or a doughnut. The physical dependence on sugar to relieve the discomfort of withdrawal reinforces the need to use more and more. The addiction grows into a real problem.” The Sugar Addict’s Total Recovery Program, Kathleen DesMaisons, Ph.D..
Dieting Reinforces Addiction
Dieting and bariatric surgery may work in a few cases when the problem is only physical. But for the majority of people, overeating is used to medicate uncomfortable feelings. In that case dieting will fail to resolve the addiction. To resolve overeating habits of binge eaters and overeaters, it is necessary to teach these individuals normal coping mechanisms for emotional stress.
Studies have shown that dieting is perceived by the brain as a restriction that challenges the homeostasis of the body. Dietary restrictions will lead the brain to want more food, to reestablish the homeostasis, whether the person weighs 300 or 100 pounds. Herein lies the failures of weight loss diets.
Mindful Awareness
The addicted mind cannot cure itself. Addictions have power over our actions because they are unconscious. Addictions will lose their power over us when we make them conscious. In order to bring unconscious thoughts and feelings to the conscious mind, we teach the practice of mindfulness. We cultivate mindfulness with habits such as walking and eating. Conscious walking consists of walking slowly with the intention to be present and observe the body rather than walking unconsciously towards a destination with a goal in mind. The goal of conscious walking is to be present to the changes and enjoy the activity of walking. With conscious eating, we develop the awareness of chewing the food, swallowing, stomach sensations and brain messages.
We apply mindful awareness to intervene with food cravings. When the binger becomes aware of his/her visualization of hyper caloric foods, he/she freezes on the spot, making his/her body still. Then the person turns their attention inward. He/she observes him/herself without judgment and with compassionate love. He/she becomes completely present to this moment connecting with his/her inner experience and accepting it. The body and the hands are not acting on the compulsion to obtain the food craved, instead the compulsion is witnessed by the higher self.
By bringing automatic unconscious reactions to consciousness, the food addict creates a space between the craving and the behavior. This space can be used to witness and understand the process that is unfolding. Take this example of Maria. Maria offers a rich description of her cravings as sensations she feels under her skin, tasting the texture of food that makes her salivate, and she goes into details about the color, consistency and appreciation of the fat content that makes the eating experience so pleasurable. She does not act on the imagery and her awareness now goes to herself and the feelings that she is trying to avoid.
Understanding the brain pathways brings detachment from the compulsion and the option to choose an alternate method besides food to deal with uncomfortable emotions. This emotional space of detachment is the opposite of compulsory. With detachment the addict can choose to let go of the compulsion. Compassionate observation and silence will bring insights into the underlying uncomfortable feelings that lead to emotional eating to the surface.